Introduction

Russell’s Viper
Russell’s viper is a highly venomous terrestrial snake of the Viperidae family. It is abundant and can be found in the Indian subcontinent, including Bangladesh, Sri Lanka, Nepal, and Taiwan, as well as in Java, mostly in open areas. This species is a significant cause of snakebite deaths within its range, as it often inhabits farmlands with frequent human contact and abundant rodent prey. The viper can grow up to about 1.5 m (5 feet) in length and is distinguished by three rows of reddish-brown spots outlined in black and white. Daboia is a live-bearer, and females commonly give birth to litters of more than 25 neonates.
- Scientific Name: Daboia russelii
- Common Names: Russell’s Viper, Chain Viper
- Geographical Distribution: Found across the Indian subcontinent, including Bangladesh.
Identification and Habitat of Russell’s Viper
- Physical Description: Heavy-bodied snake with a distinctive pattern of dark brown or black spots outlined in white or yellow.
- Habitat: Grasslands, scrub forests, and agricultural fields.
Epidemiology in Bangladesh
- Annual Incidence: Approximately 4,000 to 6,000 cases of snake bites are reported each year in Bangladesh.
- Mortality Rate: The mortality rate ranges from 1% to 3%, depending on the availability and accessibility of antivenom and healthcare facilities.
Geographical Distribution: Higher incidence in rural areas, particularly in the districts of Rajshahi, Khulna, Chittagong, and Barisal
- Incidence Rate: High incidence rates are observed in rural areas, particularly among agricultural workers.
- Seasonality: Peak incidence during the rainy season and harvest time, when human-snake encounters are more frequent.
Hospital Data on Snakebite Cases in Bangladesh
- Annual Incidence: Approximately 4,000 to 6,000 cases of snake bites are reported each year in Bangladesh.
- Mortality Rate: The mortality rate ranges from 1% to 3%, depending on the availability and accessibility of antivenom and healthcare facilities.
Clinical Presentation
- Local Effects:
- Pain and Swelling: Intense pain and progressive swelling at the bite site.
- Blister Formation: Hemorrhagic blisters may develop.
- Systemic Effects:
- Coagulopathy: Disseminated intravascular coagulation (DIC), spontaneous bleeding.
- Haemorrhage: Gastrointestinal, cerebral, or pulmonary haemorrhages.
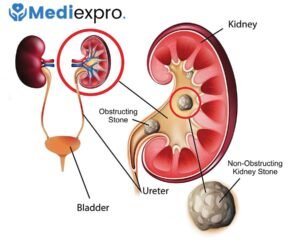
- Renal Failure: Acute kidney injury due to hemoglobinuria and myoglobinuria.
- Neurotoxicity: ptosis, ophthalmoplegia, and respiratory paralysis.
Pathophysiology
- Venom Composition: Contains proteolytic enzymes, neurotoxins, and procoagulants.
- Mechanism of Action:
- Coagulation Disruption: Activation of the coagulation cascade, leading to the consumption of clotting factors.
- Direct Tissue Damage: Proteolytic enzymes cause local tissue necrosis.
Diagnosis
- Clinical Diagnosis: Based on history of snake bite, clinical symptoms, and signs.
- Laboratory Investigations:
- Coagulation Tests: Prolonged clotting time, decreased fibrinogen levels.
- Renal Function Tests: Elevated serum creatinine and urea.
- Blood Tests: Thrombocytopenia, hematuria, myoglobinuria.
Management Strategies
First Aid
- Immediate Actions: Immobilise the affected limb, keeping the patient calm to slow the spread of venom.
- Avoidance: Tourniquets and incision/suction methods are not recommended.
Medical Treatment of Russell’s Viper Poisoning:
- Antivenom Therapy:
- Indication: All symptomatic cases should receive antivenom.
- Administration: Intravenous infusion, initial dose based on severity, with repeated premedication.
- Side Effects: Anaphylaxis, serum sickness; premedication with antihistamines may be considered.
- Supportive Care:
- Fluid Management: Intravenous fluids to maintain renal perfusion.
- Blood Products: Fresh frozen plasma, platelets, or cryoprecipitate for coagulopathy.
- Renal Support: Dialysis in cases of acute kidney injury.
- Pain Management: Analgesics for pain control.
- Monitoring:
- Vital Signs: Continuous monitoring of blood pressure, respiratory rate, and urine output.
- Laboratory Monitoring: Regular assessment of coagulation profile, renal function, and electrolyte levels.
Antivenom Therapy for Russell’s Viper Bites
Antivenom Dosage
- Initial Dose:
- Adults and Children: The initial dose is typically 10 vials of polyvalent antivenom.
- Administration: Intravenous infusion over 1 hour. Dilute the antivenom in 200-500 mL of normal saline or 5% dextrose solution.
- Assessment:
- After the initial dose, reassess the patient after 6 hours.
- Indicators for Additional Doses: Persistent or worsening symptoms such as bleeding, coagulopathy, neurotoxic signs, or renal impairment.
- Additional Doses:
- If symptoms persist, an additional 5-10 vials may be administered every 6 hours as needed.
- Continue reassessment and administration until clinical improvement is achieved and premedication is controlled.
Precautions and Preparation
- Premedication: Consider premedicating with antihistamines (e.g., chlorpheniramine 10 mg IV) and corticosteroids (e.g., hydrocortisone 100 mg IV) to reduce the risk of allergic reactions.
- Resuscitation Equipment: Ensure availability of resuscitation equipment and medications in case of anaphylactic shock.
Management of Anaphylactic Shock
Recognition of Anaphylactic Shock
- Symptoms:
- Cutaneous: Urticaria, itching, flushing, angioedema.
- Respiratory: Bronchospasm, wheezing, dyspnea, stridor.
- Cardiovascular: Hypotension, tachycardia, arrhythmias.
- Gastrointestinal: nausea, vomiting, diarrhea.
- Neurological: Dizziness, syncope, altered mental status.
Immediate Management Steps
- Stop Antivenom Infusion: Immediately discontinue the antivenom infusion if signs of anaphylaxis occur.
- Maintain Airway and Breathing:
- Airway: Ensure the airway is patent. Use airway adjuncts if needed.
- Breathing: Administer high-flow oxygen (10-15 L/min) via non-rebreather mask.
- Administer Epinephrine:
- Dosage: 0.01 mg/kg (maximum 0.5 mg) of 1:1000 (1 mg/mL) epinephrine intramuscularly, preferably in the mid-outer thigh.
- Repeat: If necessary, repeat every 5-15 minutes until improvement is noted.
- Position the Patient:
- Lay the patient flat with legs elevated if there are no signs of respiratory distress.
- If the patient is vomiting or has airway issues, place them in a recovery position.
Adjunctive Therapies
- Antihistamines:
- Diphenhydramine: 25-50 mg IV/IM.
- H2 Blockers: Ranitidine 50 mg IV may be added for additional histamine blockade.
- Corticosteroids:
- Hydrocortisone: 200 mg IV to reduce the risk of biphasic reactions and provide prolonged protection.
- Bronchodilators:
- Nebulized Albuterol: For bronchospasm, administer 2.5-5 mg of albuterol via a nebuliser.
Supportive Measures
- IV Fluids: Administer crystalloid solutions (normal saline or lactated Ringer’s) to treat hypotension and maintain blood pressure.
- Monitoring: Continuously monitor vital signs, oxygen saturation, and cardiac rhythm.
- Transfer to ICU: Consider transferring the patient to an intensive care unit for further special monitoring and management.
Follow-up Care
- Observation: Patients with anaphylaxis should be observed for at least 4-6 hours after the resolution of symptoms due to the risk of biphasic reactions.
- Education: Educate the patient about the signs of anaphylaxis and the importance of seeking immediate medical attention if symptoms recur.
Proper dosing and careful monitoring during antivenom administration are crucial for managing Russell’s viper snake bites. Preparedness to handle anaphylactic reactions can significantly improve patient outcomes. Ensuring that healthcare providers are trained in both antivenom administration and anaphylaxis management is essential in regions with high incidences of venomous snake bites.
- Improved Antivenoms: Development of more effective and specific antivenoms with reduced adverse effects.
- Biomarkers for Early Diagnosis: Research on identifying early biomarkers for coagulopathy and renal damage.
- Educational Campaigns: Community awareness programs to educate the rural population on snake prevention and first aid measures.
Public Health Perspective in Bangladesh
- Prevention Strategies: Community education on avoiding snake habitats and safe agricultural practices.
- Healthcare Access: Improving access to medical facilities and antivenom in rural areas.
- Training Programs: Regular training for healthcare providers on updated management protocols for snake bites.
Conclusion
- Summary: Russell’s viper snakebite is a significant medical emergency in Bangladesh, requiring prompt and effective management.
- Future Directions: Continued research and improved healthcare infrastructure are crucial to reducing morbidity and mortality associated with snake bites.
References
- Include recent research papers, World Health Organization (WHO) guidelines, and national health statistics on snake bites in Bangladesh.